Support from the Wisconsin Partnership Program (WPP) is enabling UW Department of Family Medicine and Community Health (DFMCH) faculty Geof Swain, MD, MPH, and Randall Brown, MD, PhD, FASAM, to launch projects to improve health outcomes for two populations: formerly incarcerated individuals re-entering the community, and people at risk for or who have opioid use disorders, respectively.
Dr. Swain: Supporting Prisoners’ Re-Entry into Society

“The hope is to improve health outcomes not only for formerly incarcerated individuals but also for their families and communities.”
—Geof Swain, MD, MPH
Dr. Swain received a five-year, $1 million grant from the WPP to reduce barriers and improve health for people returning to the community from prison.
Many formerly incarcerated individuals face major obstacles to employment, education, housing and family relationships—social determinants that are key to good health.
They also have a higher likelihood of chronic illnesses like asthma, hypertension and arthritis, and their children often have an increased risk of neglect or abuse, delinquency and poor academic performance.
Dr. Swain will collaborate with WISDOM, a group of 160 faith congregations that works for social justice and improvement of population-level health in the state.
David Liners, WISDOM’s director, considers our current system of incarceration and reentry to be “a public health problem with widespread negative health effects on people, communities and populations,” and believes that “changes could be made in the process of reintegrating non-violent offenders back into society without compromising public safety” in order to improve the health and well-being of former prisoners and their families.
Under the project, WISDOM’s ex-prisoner advocacy group, EXPO, will be expanded to train more former prisoners to provide leadership and individual mentoring. The leaders will work with prisoners re-entering society to identify and assess the biggest barriers to successfully rejoining society.
The project will also include a health-impact assessment of current and potential criminal justice policies that relate to community re-entry and crimeless parole and probation revocations.
“The ultimate goal is to improve health by improving re-entry into society and by reducing needless return to prison,” said Dr. Swain. “The hope is to improve health outcomes not only for formerly incarcerated individuals but also for their families and communities.”
Read the full story: http://www.med.wisc.edu/news-events/project-aims-to-improve-health-by-reducing-barriers-of-prisoner-re-entry-to-society/47105
Dr. Brown: Reducing Opioid Addiction Risk

“We urgently need effective means to identify risk for opioid-related complications, and interventions to prevent opioid use disorders and overdose deaths.”
—Randall Brown, MD, PhD, FASAM
Dr. Brown received a three-year, $500,000 grant from the WPP to develop an opioid risk screening tool specifically aimed at traumatic injury victims, who are at high risk for subsequent opioid addiction.
It’s part of his long-range goal to address the 300 percent increase in opioid overdoses and related deaths in Wisconsin over the past decade.
Dr. Brown will collaborate with Andrew Quanbeck, PhD, a scientist in the UW College of Engineering, and collaborators in UW Hospital’s trauma surgery group.
In the first year of the study, they will invite clinicians from Wisconsin trauma centers to a summit where they will be surveyed about practices related to opioid risk screening, potential barriers to screening and resources available to support patients with opioid use disorders.
The researchers will also recruit up to 490 traumatic-injury patients at University Hospital’s Level I Trauma Center to provide information on socio-demographics, substance use history, opioid misuse risk, mental health, medical history and injury and pain severity.
The information gathered will be the basis for development of an opioid risk screening tool to be tested at Level I and II trauma centers in Wisconsin in the third year of the project.
“Opioid addiction and overdose have reached epidemic proportions in Wisconsin and in the United States,” said Brown. “We urgently need effective means to identify risk for opioid-related complications, and interventions to prevent opioid use disorders and overdose deaths.”
Read the full story: http://www.med.wisc.edu/news-events/research-team-to-develop-and-test-opioid-risk-screening-tool/47197
Published: January 2016
The post DFMCH Faculty Lead New Projects to Help Prisoners Rejoin Society, Reduce Opioid Addiction appeared first on UW Family Medicine & Community Health.













 The UW Health Northeast Family Medical Center is helping to prevent falls among its elderly patients through increased outreach and an on-site falls prevention workshop.
The UW Health Northeast Family Medical Center is helping to prevent falls among its elderly patients through increased outreach and an on-site falls prevention workshop.

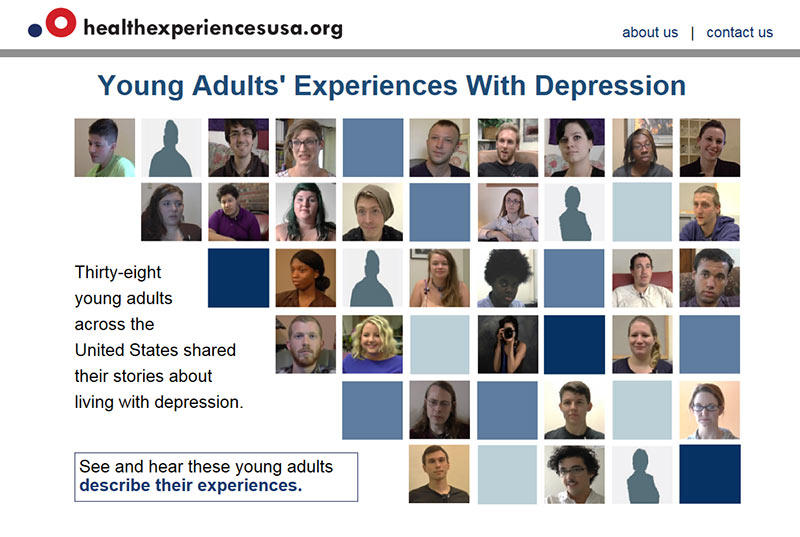 The narratives are grouped into categories such as first experiences with depression, living with depression and getting help. Specific topics within each category provide more detail.
The narratives are grouped into categories such as first experiences with depression, living with depression and getting help. Specific topics within each category provide more detail.